participate-uclh-comcov2
Participate - University College London Hospitals
Comparing COVID-19 Vaccine Schedule Combinations – Com-COV
This site is not currently recruiting
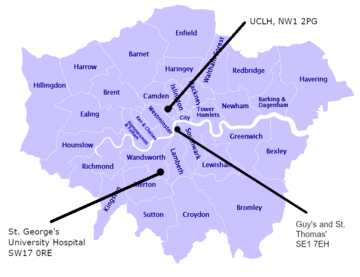
The University College London Hospitals site is recruiting participants from the London area :
What is the purpose of this research study?
There are now a number of vaccines in the UK that have been approved to prevent COVID-19, and others are expected to be approved in the near future. These use two-doses, a ‘prime’ first dose, followed by a ‘boost’ second dose some weeks later. The purpose of this trial is to see how well people’s immune systems respond when their second “boost” dose is a different type of vaccine to their first “prime” dose. We will also be looking at how common vaccine reactions, such as fever, are after such ‘mixed’ schedules. This is important, as being able to use different vaccines in this way creates a more flexible immunisation programme; potentially allowing more people to be immunised more quickly.
In this study we will be enrolling men and women aged 50 years and over who have already had one dose of a COVID-19 vaccine. We are enrolling from all ethnicities and would particularly welcome participants from the Black, Asian and Minority Ethnic (BAME) community.
What are the vaccines against?
These vaccines are against the coronavirus SARS-CoV2 that causes the disease COVID-19.
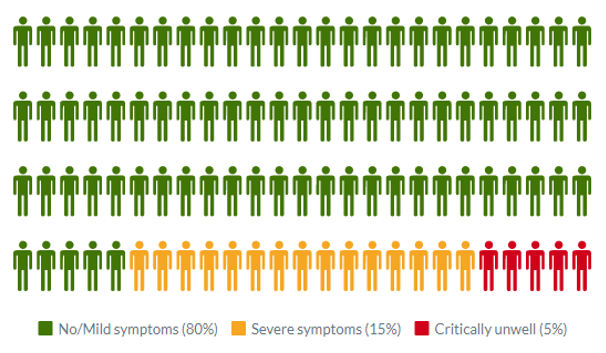
Common symptoms of COVID-19 include fever, tiredness, dry cough, and changes to taste and smell. Whilst about 80% of infected people have no or mild symptoms and will recover from the infection without needing special treatment, approximately 10-15% of cases (2-3 in 20) progress to develop severe symptoms, and about 5% (1 in 20) become critically ill.
There are some treatments that have been shown to be effective in reducing the severity of disease and the risk of death; but at present, there is no cure. Older people and those with underlying medical conditions are more likely to develop serious illness. It has also been seen that people of some ethnic groups (Black and Asian) might be at a greater risk of severe illness. More than 2.7 million people globally have died from COVID-19 as of 22nd March 2021. Some people also have symptoms that last a long time after they have recovered from the acute infection (commonly referred to as “long-COVID”). Effective vaccines can prevent infection in the first place, which is why they are so important.
Am I suitable to take part?
Adults that are aged 50 and over are able to take part. In order to be enrolled in the trial:
- You must have had your first dose of COVID-19 vaccine through the national immunisation programme between 25th January 2021 and 20th March 2021
- Be able to provide documentation of this to the trial team, or allow the trial team to check this information via NHS systems
- You must be willing to tell the trial staff about your medical history, and you may be asked to allow the trial staff to check this with your General Practitioner (GP). Bear in mind that we would also notify your GP if you joined the trial (even if we did we not need to check your medical history with them in advance).
- If you are able to become pregnant you must be willing to practice continuous effective contraception during the trial and have negative pregnancy tests on the days of vaccination
- You must agree not to donate blood during the trial
For further details on why you could not take part in this study please see the Participant Information Sheet.
Summary of the study
In this study participants will receive a second dose of a COVID-19 vaccine that may differ from their first dose received through the national immunisation programme. We are aiming to recruit 1050 participants. As new SARS-CoV-2 vaccines become available, more vaccines may be included in the trial and so the total number of participants may increase.
- Participants must be 50 years and over, and have had one dose of a COVID-19 vaccine through the national immunisation programme approximately 8 to 12 weeks before being enrolled in the study. They cannot have received their boost dose already.
- Participants will be allocated, at random, to receive the same vaccine as their first dose “prime”, or one of two different COVID-19 vaccines.
- They will not know which vaccine they have received for their boost (i.e. they will be “blinded”)
- Between 5 and 7 routine blood tests will be taken over 10 months to look at the immune responses to the vaccine depending on the group you are in. You may also be asked for a nasal fluid and saliva sample at each visit. You might also be asked to attend for a repeat blood test if there were any safety concerns.
- Participants will need to complete an online diary for up to 28 days following the vaccine received in the trial
- Participants should expect their involvement in the trial to last approximately 10 months
- We would not be offering diagnostic COVID-19 testing as part of this trial, but it is important that participants in this trial access COVID-19 testing outside of the trial following normal government guidance.
- If you were to test positive for the virus causing COVID-19 we may ask you to attend for an extra visit.
Once you have received your vaccine through the trial, unless specifically advised by us, you would not be eligible to receive any further vaccine dose via the government vaccination scheme. This will be reviewed if government guidance changes.
What vaccines are being used in this study?
At present, the vaccines in this trial are:
- Oxford/AstraZeneca ChAdOx1 nCoV-19 (hereafter referred to as AstraZeneca)
- Pfizer/BioNTech BNT162b2 (hereafter referred to as Pfizer)
- COVID-19 Vaccine Moderna (hereafter referred to as Moderna)
- Novavax NVX-CoV2373 (hereafter referred to as Novavax)
Pfizer, Moderna, and AstraZeneca vaccines have been approved for emergency use in the UK under regulation 174 of the Human Medicines Regulations 2012.
The vaccine Novavax has been tested in clinical trials that have enrolled over 45 000 people, and has been shown to be highly effective at preventing COVID-19. This vaccine has not yet been approved for use by the UK Medicines Healthcare Regulatory Agency (MHRA), but this process is ongoing.
The potential schedule of how the vaccines would be given is detailed below.
|
Vaccine received in routine Immunisation Programme |
Trial boost vaccine – one of the following options 8-12 weeks from first vaccine |
|
Approximately 525 participants in each group |
Approximately 175 participants in each group |
|
AstraZeneca |
AstraZeneca |
|
Moderna |
|
|
Novavax |
|
|
Pfizer |
Pfizer |
|
Moderna |
|
|
Novavax |
AstraZeneca
This vaccine has been tested in more than 20,000 people worldwide and has been found to be both safe, and effective in preventing COVID-19.
The AstraZeneca vaccine is made from a virus (ChAdOx1), which is a weakened version of a common cold virus (adenovirus). This has been genetically changed so that it is impossible for it to grow in humans. Added to this virus is a small amount of the genetic coding material of the SARS-CoV-2 spike (S) protein, which plays an essential role in SARS-CoV-2 infection. Your cells then start producing the SARS-CoV-2 spike protein. Your immune system then “sees” these spike proteins, and makes a protective immune reaction against them that helps stop SARS-CoV-2 infections.
Pfizer
This is a messenger RNA (mRNA) vaccine. This vaccine uses a small amount of the genetic coding material (mRNA) of the SARS-CoV-2 spike (S) protein packaged inside very small fatty particles (lipid nanoparticles). When these are injected into your body, your cells take up these fatty particles, and then start producing the SARS-CoV-2 spike protein. Your immune system then “sees” these spike proteins, and makes a protective immune reaction against them. The original mRNA that has been taken into your cells is broken down within a few days, and cannot be incorporated into your own genetic code.
This vaccine has been tested in more than 40,000 people worldwide and has been shown to be both safe, and effective in preventing COVID-19.
Moderna
This is also an mRNA vaccine, so works in a similar way to the Pfizer vaccine. This vaccine has been tested in more than 30,000 people worldwide, and has been shown to be both safe and effective in preventing COVID-19
Novavax
This vaccine is based on the spike protein from the SARS-CoV-2 virus in combination with an adjuvant, a substance that increases the response of the immune system to the protein. The adjuvant is called “Matrix-M1™” and consists of saponin (which is derived from the soapbark tree) and natural fats.
None of these vaccines contain live SARS-CoV-2 coronavirus and therefore cannot give you COVID-19.
What are the side effects of these vaccines?
Common side effects
People very often have tenderness, pain, warmth, redness, itching, swelling or bruising or less commonly have a small lump in their arm where they have been vaccinated.
Other common systemic side effects
Some people can develop these symptoms after vaccination. They usually last for less than a week after you are vaccinated (more commonly 24-48 hours afterwards).
- Fatigue
- Headaches
- Flu-like symptoms, such as high temperature, sore throat, runny nose, cough and chills
- Muscle aches
- Joint aches
- Feeling unwell (malaise)
- Feeling sick or nauseated or vomiting
Other less common side effects:
- Abdominal pain
- Decreased appetite
- Feeling dizzy
- Swollen lymph nodes (glands)
- Excessive sweating, itching skin or rash
- Rashes
Many of these symptoms can be reduced by use of paracetamol around the time of immunisation and over the next 24 hours. We would not routinely recommend the use of ibuprofen or other anti-inflammatory medication at this time.
After immunisation with the Pfizer vaccine, difficulty sleeping has been observed in fewer than 1 in 100 people, and weakness of the muscles on one side of the face has been observed in fewer than 1 in 1000 people.
What are the advantages of taking part?
We anticipate that participating in the trial will mean that you gain some protection against the coronavirus (but cannot guarantee this). You may also receive your boost dose of vaccine a few weeks earlier than you were planned to receive it from the national immunisation programme. Most importantly, the information gained from the trial will make a valuable contribution to the pandemic response.
Are there any risks from taking part in the study?
In addition to the potential side effects of the vaccines outlined above, the blood samples taken in the study may cause slight pain and occasionally bruising. Please refer to the Participant Information Sheet for full details of procedures and potential risks.
What will happen if I don’t want to carry on with the trial?
If, at any time after agreeing to participate, you change your mind about being involved with this study you are free to withdraw without giving a reason. If you withdraw we would not usually perform any more research procedures, although occasionally we might need to offer you a follow up visit for safety purposes, for example to check the injection site or a blood result. Your decision will not result in any penalty. Unless you state otherwise, any samples taken whilst you have been in the study will continue to be stored and used for research as detailed above. You are free to request that your samples are destroyed at any time during or after the study. If you choose to withdraw from the trial, your standard medical care will not be affected.
What’s next?
If you would like to find out more, please read the Participant Information Sheet and if you are interested in taking part, please complete our pre-screening questionnaire.
Download the Participant Information Sheet (PDF)
This site is not currently recruiting
Complete the Pre-screening Questionnaire
For further details contact us on :




